Smart open-up of OPDs during COVID-19 pandemic and beyond

As the lock down is ending in the country, Ifeel obliged to write this article on the essential precautions doctors need to take while re-starting their OPD to ensure smooth and safe functioning of their practice.
Many of us have drastically reduced the number of patients we see daily. While some of us have completely stopped seeing patients in the OPD, while some are conducting net-based telemedicine visits from our offices or virtual-visits from home. In a recent US survey 42% of health-care establishments has laid off their staff (and many have taken up salary cuts); 20% of primary health services are completely closed off (perhaps permanently).
The situation in our region is not clear but most like to beworse than this. We are all hoping that the peak of the COVID-19 pandemic will quickly pass and numbers will start declining so that we can open up our practices.
The American Medical Associationhas actually proposed 4 goal-posts to be achieved before OPD services could be restarted:
- Minimal risk of community transmission based on sustained evidence of a downward trend in new cases and fatalities
- A robust, coordinated, and well-supplied testing network
- A public health system for surveillance and contact tracing
- Fully resourced hospitals and healthcare workforce
However, unfortunately for us, the COVID-19 numbers continue to escalate with no end-of-the-tunnel in sight. It seems that we will have to “smart re-open” our OPD practice in the near future the above goal-posts and despite the paucity of the testing kits. At the same time, we realize that our practice probably won't be the same as before. It seems that the practice will now changefundamentally The primary principle of practice will be to keep patients and healthcare workers safe.
What are the foreseeable changes?
Changes in the clinical practice:
- Face-to-face time with patients should be limited. Regular follow-up visits just for the sake of periodic monitoring should be decreased. Interval appointments or ‘follow-up' will be replaced by online 'virtual visits'.
- Prioritizecare and evaluate the necessity of the care based on clinical needs.
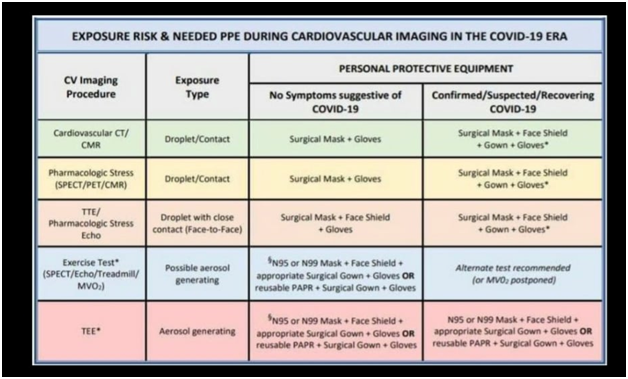
- Use preventive strategies as much as possible including PPE as per need
- Health-care practitioners (HCPs) will have to be more acceptable and conversant with smartphones and its apps, smart-watch, and monitoring devices (Fitbit), video conferencing such as skype, zoom etc.
- Make a plan: Pre-opening plan and date is critically important. Ideally, a period of 'soft-reopening' would be fine.
- Assess your personal protective equipment (PPE) needs and place the necessary orders.
- Set up standard operating procedures (SOPs); staffing and cleaning, isolation/quarantine if an employee or patient is diagnosed with COVID-19 after being in the clinic.
- Open incrementally: Consider a step-wise approach to reopening so that the practice may quickly identify and address any practical challenges.
- Identify what visits are really required and what can be done via telemedicine. Begin with a few in-person visits a day, and then keep on incrementally increasing.
- Remote monitoring abilities should be utilized more, instead of in-person checks for vital signs, such as respiratory rate, oxygenation, blood glucose levels, heart rate. Electronic BP machine and infra-red thermal guns are to be preferred.
Certain Changes in clinics
- Limit the number of patients in the waiting room: Patients/accompanying person may be asked to wait elsewhere (maybe car/lobby) till their allotted number is called.
- Limit the number of accompanying person to the clinic: Post the changed OPD policy at the clinic/OPD entrance and also on the clinic's website.
- Maintain social distancing in the waiting room.
- Consider a flexible schedule, with more time in between patient visits.
- Shared objects like magazines or toys have to be done away with. Instead, install video content.
- Hand sanitizers and the wearing of masks have to be made mandatory.
- Staircase and door handles need to be cleaned regularly
- Screen patients/care-givers. Temperature monitoring of patients/care-takers has to be undertaken before they enter the clinic premises and patients should be enquired about presence of COVID symptoms.
- Dedicated schedule and different room should be allocated for patients with respiratory/fever/symptoms suggestive of COVID-19. These patients should be examined utilizing the full PPEs and other protective equipment. The rooms should be thoroughly sanitized in between visits and after these exams are done.
- Co-ordinate COVID testing with appropriate centers. Many health systems have instituted the practice of testing all patients who are being scheduled for elective or high-intensity procedures (such as outpatient surgeries or services requiring close contact including dental).
- All others who work in the clinic should be routinely screened for high temperature and other symptoms of COVID-19 including olfactory test.
- Staff schedules will need to be adjusted on rotating basis with 2or 3 groups each group covering a week or so and they should be instructed not to attend clinic if they have any symptoms of COVID.
- Keep adequate social distancing between employees and develop protocols for sharing spaces (e.g. kitchens, bathrooms, canteens, reception)
Change patient expectations:
- Patients will also be more comfortable with ‘remote’ examination once they know that it is safer for them too. Patients should be counseled and convinced that telecommunication is safe and effective.
Change in financial re-imbursement:
- The way payments are made would also be changed. There will be more of online payments (bank transfers,ePay, eSewaetc)
- For lone-workers it may be a good idea to join some larger group temporarily.
Legal implications:
- New legal issues and obligations may arise as the practice reopens.
- Legal implication of telemedicine will have to be re-worked in light of need for social distancing















